Responsive Feeding Clinical Paper Summary - Prevention of Childhood Obesity
Do bottle-fed infants lack self-regulation of milk intake compared with directly breastfed infants?1
Why it’s important
The prevention of childhood obesity is becoming a global public health priority. Feeding practices in the first year of life have been reported to affect growth and body composition, with breastfed infants gaining less weight than formula-fed infants and having less risk of overweight and obesity for later childhood.
Aim and method
There were 2 hypotheses:
- Infant weight gain is not only affected by type of milk but also by mode of milk delivery
- Regardless of the type of milk in the bottle, bottle feeding might put infants on a faster track of weight gain
The paper looked at whether the infant was receiving breast milk, formula milk or a combination and also how the infant was being fed – by breast or by bottle.
Key findings
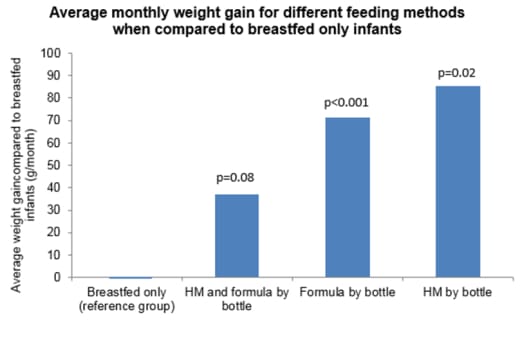
Infants fed breast milk in a bottle grew faster than those who were breastfed. This may be due to the fact that infants who are bottle fed (regardless if formula or breast milk) find it harder to self-regulate than if they were at the breast and because the caregiver establishes a more controlling behaviour of feeding, i.e. giving the child every drop in the bottle and maybe not recognising the infant’s internal cues of hunger and satiety.
Breastfed infants play a more active role in determining their milk intake. Feeding cues are also interpreted more effectively, compared to infants who are bottle fed.
Summary
The authors state that breastfeeding and breast milk are fundamentally different. This study suggests that bottle feeding, regardless of the milk in the bottle (i.e. breast milk or formula milk), may be an independent factor associated with infant weight gain.
Infants that are bottle-fed may gradually lose their ability to self-regulate and ultimately gain weight faster than those infants who are breastfed – as baby-led feeding is more commonly practiced when bottle-feeding infants. Special attention is needed for infants’ cues of hunger and satiety when bottle feeding and can play a big part in the prevention of childhood obesity.
Related Articles
-
Li R et al. Pediatrics 2010; 125: e1386–e1393.
IMPORTANT NOTICE:
The World Health Organisation (WHO) has recommended that pregnant women and new mothers be informed on the benefits and superiority of breastfeeding – in particular the fact that it provides the best nutrition and protection from illness for babies. Mothers should be given guidance on the preparation for, and maintenance of, lactation, with special emphasis on the importance of a well-balanced diet both during pregnancy and after delivery. Unnecessary introduction of partial bottle-feeding or other foods and drinks should be discouraged since it will have a negative effect on breastfeeding. Similarly, mothers should be warned of the difficulty of reversing a decision not to breastfeed. Before advising a mother to use an infant formula, she should be advised of the social and financial implications of her decision: for example, if a baby is exclusively bottle-fed, more than one can (400 g) per week will be needed, so the family circumstances and costs should be kept in mind. Mothers should be reminded that breast milk is not only the best, but also the most economical food for babies. If a decision to use an infant formula is taken, it is important to give instructions on correct preparation methods, emphasising that unboiled water, unsterilised bottles or incorrect dilution can all lead to illness.