Frequently asked questions about vitamin D for babies
Overview
Vitamin D is a fat-soluble vitamin and an essential nutrient. It supports healthy bone development and vital functions such as the immune system from conception through childhood and into adulthood1.
The Department of Health and Social Care recommends that from birth to 1 year of age, breastfed babies should receive vitamin D supplements to make sure they get enough2.
What are the benefits of Vitamin D for babies?
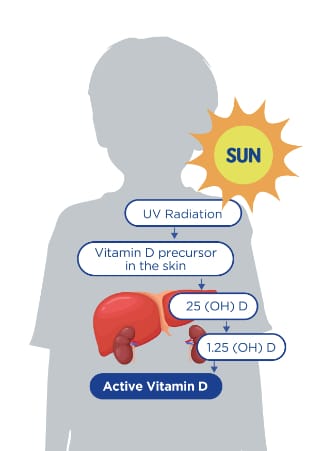
Vitamin D is a prohormone that enters the body through a precursor in the skin, it is then transformed into its active form in the liver and kidneys. Direct sunlight exposure is the best source of natural vitamin D, it is synthesized in the skin upon exposure to sunlight containing sufficient Ultraviolet B (UVB) radiation, levels of which are higher in the summer months, around midday. This is the main source for most people. It can also be obtained from foods or vitamin D supplements.
Vitamin D is synthesised in the skin by the action of sunlight containing UBV radiation (April to September).
Vitamin D deficiency can lead to fits or rickets3,4, dietary sources are essential when sunlight containing UVB radiation is limited (for example, during the winter months). There are specific recommendations for supplementation, these consist of vitamin D drops for babies.
People with more skin pigment absorb less UVB than those with fair skin and will need more sun exposure to produce the same amount of vitamin D5. To ensure a healthy status during winter months is important to take a vitamin D supplement6-8.
What are the dietary sources of Vitamin D?
Vitamin D is found in a small number of foods such as:
- Oily Fish
- Organ meat, such as liver
- Egg yolks
- Milk
- Fortified foods like breakfast cereals and fat spreads9
How much vitamin D per day is recommended for babies and children?
Babies and young children are at risk of developing vitamin D deficiency8. Body stores can decline by 50% over less than a month in infants, and thus without a source of vitamin D, vitamin D deficiency can rapidly develop1.
A ’safe intake’ of 5μg/d of vitamin D is recommended for all infants from birth up to 1 year (whatever their mode of feeding) in Ireland.
Vitamin D for breastfed babies
The Department of health recommends that babies who are being breastfed are given a daily vitamin D supplement from birth, whether the mother is taking the supplement herself or not. Vitamin D for breastfed babies: From birth to 1 year, breastfed babies should be given a daily supplement containing 5 micrograms (µg) of vitamin D2.
Vitamin D for formula-fed babies
Infants who are formula-fed should be given a vitamin D supplement if they're having less than 500ml (about a pint) of infant formula a day, as infant formula is fortified with vitamin D and other nutrients2.
How much vitamin D per day should be taken during toddlerhood?
The National Preschool Nutrition Survey (NPNS) showed that almost 80% of children age 1-4 years have poor vitamin D intakes10.
Children aged 1 to 4 years old should be given a daily supplement containing 5µg of vitamin D, especially in winter months11.
Summary
The Department of Health in Ireland recommends2:
- Breastfed babies from birth to 1 year of age, should be given a daily supplement containing 5ug of vitamin D.
- Formula-fed babies should not be given a daily vitamin D supplement if they are having more than 300ml of infant formula a day. This is because infant formula is fortified with vitamin D.
- Children aged 1 to 4 years old should also be given a daily supplement containing 5ug of vitamin D during the winter months.
Educating parents and carers about the importance of vitamin D is important to help improve the supplement adherence rates in Ireland.
Watch the 1-minute video below for a summary.
-
Vitamin D supplementation for infants. Available at https://www.who.int/elena/titles/bbc/vitamind_infants/en/ (Accessed September 2021)
-
Vitamins for children. NHS, 2021. Available at https://www.nhs.uk/conditions/baby/weaning-and-feeding/vitamins-for-children/ Accessed September 2021.
-
Uday S, et al. Variations in infant and childhood vitamin D supplementation programmes across Europe and factors influencing adherence. Endocrine connections 2017;6:667-75
-
Day RE, et al. We still don’t know that our children need vitamin D daily: a study of parents’ understanding of vitamin D requirements in children aged 0-2 years. BMC Public Health 2019; 19:1119
-
NICE. Vitamin d deficiency in children. December 2016. Available at https://cks.nice.org.uk/vitamin-d-deficiency-in-children Accessed August 2021
-
SACN report on Feeding in the first year of life. Available at https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/725530/SACN_report_on_Feeding_in_the_First_Year_of_Life.pdf (Accessed September 2012)
-
Lennox A, Sommerville J, Ong K, et al. 2013. Diet and nutrition survey of infants and young children, 2011.
-
Food fact sheet, Vitamin D, BDA. Available at https://www.bda.uk.com/uploads/assets/01d7715f-c4f7-42e7-96f67018f035b0ea/Vitamin-d-food-fact-sheet.pdf. (Accessed September 2021)
-
NHS. The new guidelines on vitamin D – what you need to know. Available at: https://www.nhs.uk/news/food-and-diet/the-new-guidelines-on-vitamin-d-what-you-need-to-know/ (accessed September 2021).
-
The National Pre-School Nutrition Survey Summary Report (2012). Food and Nutrient Intakes, Physical Measurements and Barriers to Healthy Eating. Irish Universities Nutrition Alliance.
-
Vitamin d for babies 0 to 12 months. Available at https://www2.hse.ie/wellbeing/child-health/vitamin-d-for-babies-0-12-months.html (Accessed September 2021)
IMPORTANT NOTICE:
The World Health Organisation (WHO) has recommended that pregnant women and new mothers be informed on the benefits and superiority of breastfeeding – in particular the fact that it provides the best nutrition and protection from illness for babies. Mothers should be given guidance on the preparation for, and maintenance of, lactation, with special emphasis on the importance of a well-balanced diet both during pregnancy and after delivery. Unnecessary introduction of partial bottle-feeding or other foods and drinks should be discouraged since it will have a negative effect on breastfeeding. Similarly, mothers should be warned of the difficulty of reversing a decision not to breastfeed. Before advising a mother to use an infant formula, she should be advised of the social and financial implications of her decision: for example, if a baby is exclusively bottle-fed, more than one can (400 g) per week will be needed, so the family circumstances and costs should be kept in mind. Mothers should be reminded that breast milk is not only the best, but also the most economical food for babies. If a decision to use an infant formula is taken, it is important to give instructions on correct preparation methods, emphasising that unboiled water, unsterilised bottles or incorrect dilution can all lead to illness.